Sleep is a vital component of our overall health, yet many of us take it for granted. Among the various sleep disorders, obstructive sleep apnea (OSA) is one of the most common, affecting millions worldwide. In this post, we will delve into what OSA is, its symptoms, causes, diagnosis, and treatment options, while raising awareness about its impact on overall well-being.
What is Obstructive Sleep Apnea?
Obstructive sleep apnea is a serious sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions occur when the throat muscles relax excessively, leading to a blockage of the airway. As a result, the brain and body experience oxygen deprivation, leading to various health issues.
How OSA Works
During sleep, the muscles in the throat relax. In people with OSA, these muscles relax too much, leading to a partial or complete blockage of the airway. This blockage can cause snoring and choking sensations, leading the person to wake up repeatedly throughout the night to catch their breath. This disruption prevents them from entering the deeper stages of sleep, leading to significant daytime fatigue and other health complications.
Symptoms of Obstructive Sleep Apnea
Recognizing the symptoms of OSA is crucial for early intervention and treatment. Some common symptoms include:
- Loud Snoring: Often the most noticeable sign, loud snoring is common in individuals with OSA.
- Choking or Gasping During Sleep: This is usually witnessed by a bed partner and indicates the person is struggling to breathe.
- Excessive Daytime Sleepiness: Individuals may feel excessively tired during the day, making it difficult to focus or stay awake.
- Morning Headaches: Due to oxygen deprivation during the night, many people wake up with headaches.
- Mood Changes: OSA can contribute to irritability, anxiety, and depression.
- Difficulty Concentrating: Lack of restorative sleep can lead to impaired cognitive function.
- Dry Mouth or Sore Throat: Frequent awakenings may lead to a dry mouth or sore throat in the morning.
Causes and Risk Factors
Understanding the causes and risk factors associated with OSA is essential for prevention and management. Some common causes include:
1. Obesity:
- One of the leading risk factors for OSA, excess body weight can contribute to the narrowing of the airway. A significant percentage of OSA patients are overweight or obese.
2. Age:
- OSA can occur at any age but is more common in middle-aged adults. As people age, the muscle tone in the throat decreases, increasing the risk.
3. Gender:
- Men are more likely to develop OSA than women. However, the risk for women increases after menopause.
4. Family History:
- A family history of sleep apnea can increase an individual’s risk of developing the condition.
5. Alcohol and Sedative Use:
- Alcohol and sedatives can relax the throat muscles, worsening the symptoms of OSA.
6. Smoking:
- Smoking can increase inflammation and fluid retention in the upper airway, contributing to breathing problems during sleep.
7. Nasal Congestion:
- Individuals with chronic nasal congestion or allergies may have an increased risk of developing OSA.
8. Medical Conditions:
- Certain medical conditions, such as high blood pressure, diabetes, and heart conditions, can increase the risk of OSA.
The Impact of OSA
The prevalence of OSA is on the rise, primarily due to increasing rates of obesity and sedentary lifestyles. Many people remain undiagnosed and unaware of the condition, which can lead to various health complications.
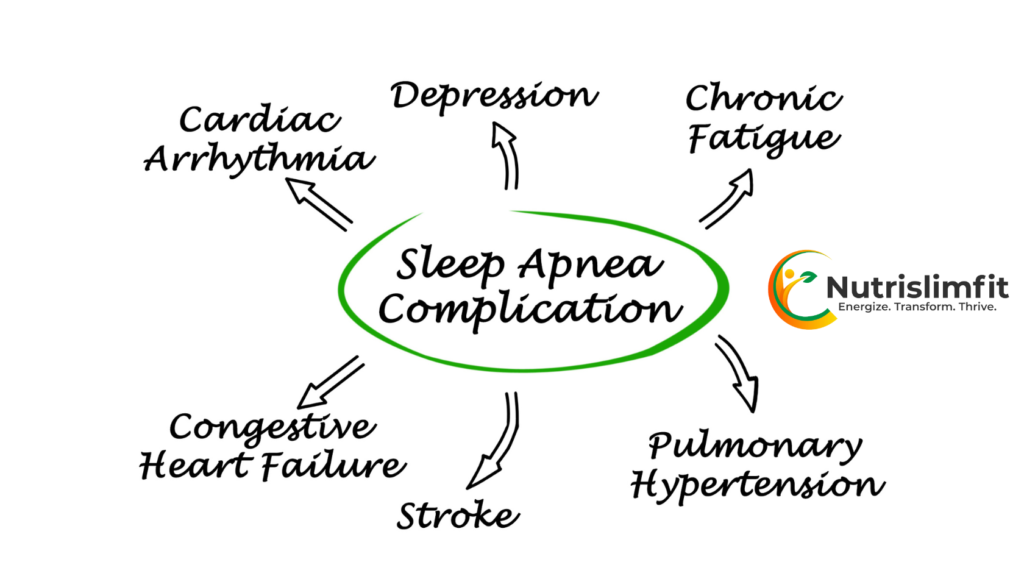
Health Consequences
The impact of untreated OSA extends beyond sleep disturbances. It can lead to various health complications, including:
- Cardiovascular Issues: OSA is linked to hypertension, heart attacks, and stroke.
- Type 2 Diabetes: The condition can exacerbate insulin resistance and glucose intolerance.
- Metabolic Syndrome: OSA is associated with weight gain and metabolic issues, increasing the risk of metabolic syndrome.
- Liver Problems: Fatty liver disease is more prevalent among OSA patients.
- Mental Health Disorders: Anxiety and depression can be exacerbated by sleep disturbances caused by OSA.
Diagnosis of Obstructive Sleep Apnea
Diagnosing OSA involves a combination of medical history evaluation, symptom assessment, and sleep studies. Here’s a breakdown of the diagnostic process:
1. Medical History and Physical Examination:
- A healthcare provider will review the patient’s medical history, sleep patterns, and any associated symptoms. They may also perform a physical examination to check for signs of OSA, such as obesity and nasal congestion.
2. Sleep Studies:
- Polysomnography (PSG): This is the gold standard for diagnosing OSA. Conducted overnight in a sleep clinic, PSG records brain waves, oxygen levels, heart rate, and breathing patterns.
- Home Sleep Apnea Testing (HSAT): In some cases, home tests may be prescribed to monitor breathing and oxygen levels during sleep.
3. Questionnaires:
- Tools like the Epworth Sleepiness Scale can help assess the level of daytime sleepiness and the likelihood of OSA.
Treatment Options for OSA
The treatment for obstructive sleep apnea varies depending on the severity of the condition and individual patient needs. Here are some common treatment options:
1. Lifestyle Changes:
- Weight Loss: Losing even a small amount of weight can significantly improve symptoms in overweight individuals.
- Exercise: Regular physical activity can help reduce symptoms and improve overall health.
- Positional Therapy: Some individuals benefit from sleeping on their sides instead of their backs, which can help keep the airway open.
2. Continuous Positive Airway Pressure (CPAP):
- The most common treatment for moderate to severe OSA, CPAP involves wearing a mask connected to a machine that delivers continuous air pressure to keep the airway open during sleep.
3. Oral Appliances:
- Dental devices can help reposition the jaw and tongue to keep the airway open. These are particularly useful for individuals with mild to moderate OSA or those who cannot tolerate CPAP.
4. Surgery:
- In certain cases, surgical options may be considered to remove excess tissue or correct structural abnormalities in the airway. Common surgical procedures include uvulopalatopharyngoplasty (UPPP), maxillomandibular advancement (MMA), and radiofrequency ablation.
The Role of Awareness and Education
Awareness about obstructive sleep apnea remains low. Many individuals suffering from OSA may not recognize their symptoms or may dismiss them as mere fatigue. Education plays a crucial role in encouraging individuals to seek medical advice and undergo appropriate testing.
1. Community Outreach:
- Healthcare providers can play a pivotal role by conducting workshops and seminars to educate communities about the signs and risks associated with OSA.
2. Collaborative Efforts:
- Collaboration between healthcare professionals, sleep specialists, and general practitioners can help streamline the referral process for patients suspected of having OSA.
3. Utilizing Technology:
- Telemedicine and mobile health applications can aid in monitoring symptoms and facilitating consultations, especially in areas where access to healthcare may be limited.
Conclusion
Obstructive sleep apnea is a significant public health concern with far-reaching consequences on individual health and productivity. Understanding its symptoms, causes, and treatment options is vital for early detection and effective management. By increasing awareness, promoting healthy lifestyles, and advocating for proper diagnosis and treatment, we can work towards reducing the impact of OSA in our communities.
If you or someone you know exhibits signs of obstructive sleep apnea, it’s essential to seek professional help. Remember, a good night’s sleep is not just a luxury; it is a necessity for a healthier and more fulfilling life. Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before making any decisions regarding your health or before using any medications.
And for Sports Nutrition for Athletes click here


